What Are Percs? Percocet Abuse Risks & Effects
Percocet, often called “Percs,” might seem like a quick fix for pain relief, but the hidden risks can spiral into addiction, health damage, and life-altering consequences.
Percocet is a prescription painkiller that combines two ingredients: oxycodone, a powerful opioid, and acetaminophen, a common over-the-counter pain reliever. Doctors usually prescribe it for short-term pain after surgery or injury. But the relief it brings can quickly become a trap.
Because oxycodone affects the brain’s reward system, it doesn’t just dull pain—it creates a wave of calm, sometimes euphoria. That’s why so many people slip from medical use into misuse. And when that happens, things escalate fast.
This article breaks down what Percocet abuse is, why it’s risky, and how you—or someone you care about—can find a way out.
What Are Percs? A Closer Look at Percocet
“Percs” is street slang for Percocet, and if you’re hearing it more often, you’re not alone. Percocet has been making the rounds far beyond doctor’s offices and pharmacies because it’s a form of opioid that’s used to treat pain.
Oxycodone, the main active ingredient, changes how the brain interprets pain. But it also interferes with dopamine levels—the chemical that makes you feel good. That elation, while short-lived, is what hooks people in.
It doesn’t take long to start needing more to feel the same effect. Before you know it, chasing relief becomes a full-time job.
The Dangers of Percocet Abuse
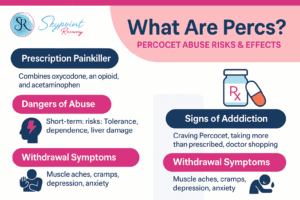
Percocet abuse poses significant risks to physical, mental, and social well-being.
Short-Term Risks
Even at prescribed doses, Percocet comes with baggage. Drowsiness, nausea, vomiting, constipation, and slowed breathing are just the beginning. Add misuse to the mix and those effects can tip into dangerous territory quickly.
Long-Term Consequences
Over time, the body builds a tolerance. That means more pills just to get through the day. Then comes dependence. Eventually, Percocet stops being about feeling good—it’s about not feeling awful.
Mentally, the impact can be brutal. Depression, anxiety, even suicidal thoughts can creep in. And that’s without counting the damage to your liver and kidneys from prolonged acetaminophen use. Overdose isn’t a rare occurrence. In fact, almost 80% of the world’s 600,000 drug overdose deaths in 2019 are related to opioids.
Social and Lifestyle Impacts
Percocet doesn’t just affect the body and mind. It seeps into every part of life. Maybe it starts with missing a meeting or forgetting a promise. But soon, relationships crumble, jobs vanish, and finances fall apart. It’s not just a drug problem—it’s a life problem.
Signs of Percocet Addiction
Spotting addiction isn’t always easy, especially when someone is trying hard to hide it. But there are clues:
- Craving Percocet, even when pain is gone
- Taking more than prescribed—or lying to get more
- Doctor shopping to maintain the supply
- Missing work, skipping obligations, or withdrawing from loved ones
- Physical signs like sweating, trembling, nausea, or insomnia when not using
If these sound familiar, it’s time to take a hard look at what’s going on.
Percocet Withdrawal: Challenges in Quitting
Stopping Percocet after developing dependence brings intense withdrawal symptoms. The body has adapted to the drug’s presence and reacts strongly when it’s removed.
Physical Symptoms
When the body’s dependent, quitting is no picnic. Expect muscle aches, cramps, diarrhea, chills, and insomnia. It’s not just uncomfortable—it’s overwhelming.
Psychological Symptoms
Then there’s the mental side: depression, anxiety, and a crushing sense of hopelessness. Many people relapse just to make those feelings stop.
Why Quitting Alone Might Not Be Safe
It might seem brave to go cold turkey, but it’s risky. Withdrawal symptoms can be severe, and without support, the odds of long-term success are slim. Professional help offers a safer—and more successful—way forward.
How Skypoint Recovery Can Help
Recovery isn’t one-size-fits-all. That’s why Skypoint Recovery in Akron, Ohio offers a range of personalized options.
Comprehensive Programs
Depending on your needs, you might start with a Partial Hospitalization Program (PHP) or step into an Intensive Outpatient Program (IOP) that lets you keep up with life while getting serious care. Transitioning out? Our sober living homes in Akron provide structure and support during early recovery.
Dual Diagnosis Treatment
Many people dealing with Percocet addiction also face anxiety, depression, or trauma. Skypoint’s dual diagnosis treatment helps uncover and treat both issues together, so healing actually sticks.
Personalized Care
No judgment, no cookie-cutter plans—just substance abuse counseling that meets you where you are. Whether you need painkiller addiction help or support for prescription drug abuse, the team will walk with you every step of the way.
They accept Medicaid and will help you figure out financial options that work.
Taking the First Step Toward Recovery
If you’re struggling—or watching someone you love disappear into opioid use—it’s time. You don’t need to hit rock bottom to ask for help.
The team at Skypoint Recovery is ready to help you find the right program and start healing. Call 855-612-3488 or fill out our online form to get started. There’s no pressure—just a chance to start feeling like yourself again.
Breaking Free from Percs
Percocet abuse is a serious issue with devastating consequences. But addiction isn’t a life sentence. Recovery is possible. By understanding the risks, recognizing the signs, and seeking professional help, you can break free from the grip of Percs and reclaim your life. Skypoint Recovery in Akron, OH, is ready to help you on that journey.
If you or someone you know is struggling, don’t hesitate. Reach out to Skypoint Recovery today. You can fill out our online form or call us at 855-612-3488. There is hope, and there is help.




















